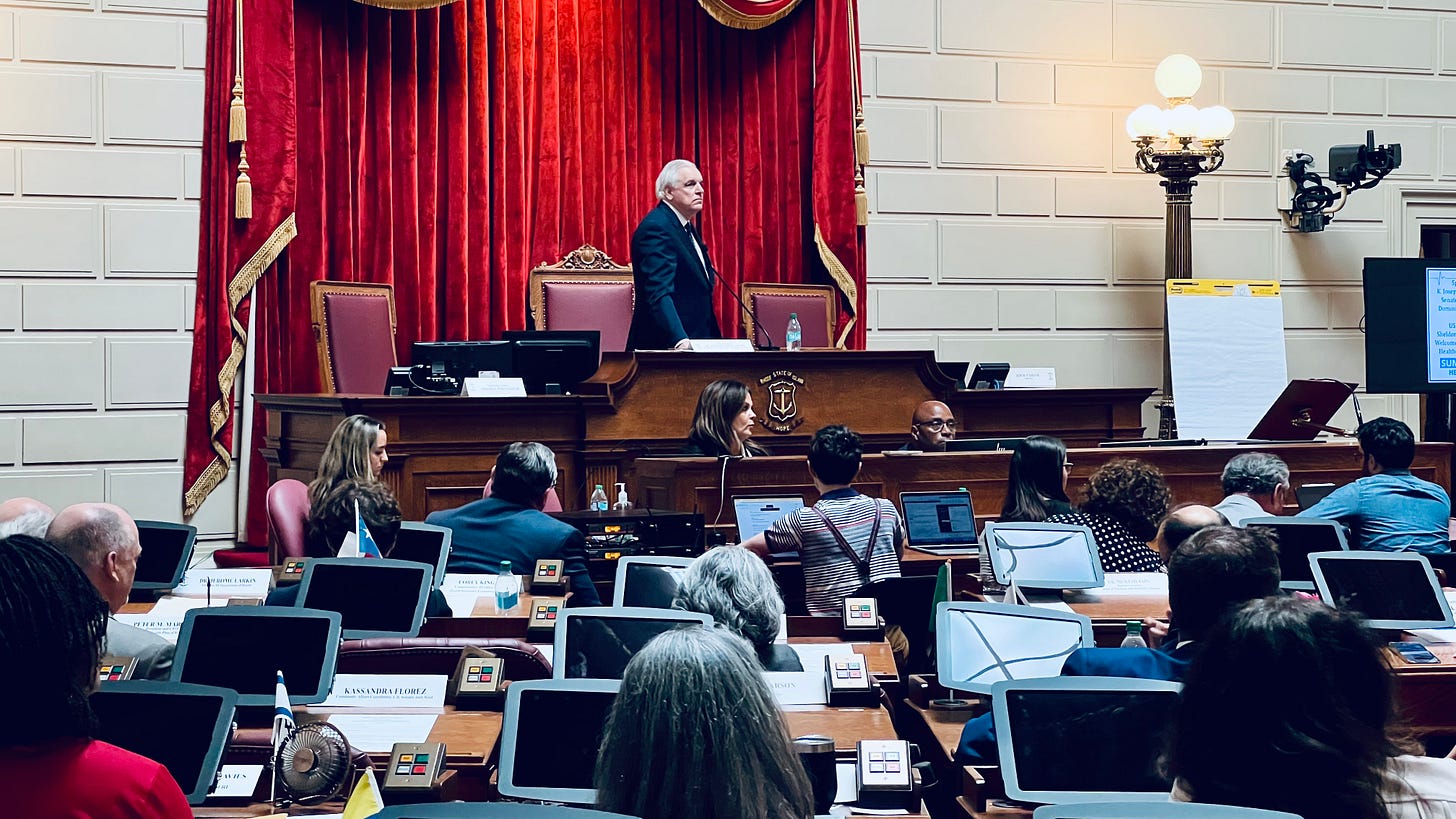
Sharp divides and few answers at Tuesday morning's Healthcare Summit
"...make no mistake, we need change," said Rhode Island Attorney General Peter Neronha.
United States Senator Sheldon Whitehouse (Democrat, Rhode Island) was the keynote speaker at Tuesday morning's summit on the current state of Rhode Island’s healthcare system organized by House Speaker Joseph Shekarchi and his staff.
The summit brought together healthcare physicians and providers, hospital CEOs, industry leaders, insurers, and other pivotal stakeholders to engage in a comprehensive discussion on the issues. Topics included the strengths and weaknesses of Rhode Island's existing delivery system, insurance programs, workforce and educational requirements, and equitable access to affordable, quality care.
Some clear lines of disagreement were visible. Senator Whitehouse expressed disappointment in the failure of the Lifespan/Care New England merger, which was blocked in part by the efforts of Rhode Island Attorney General Peter Neronha. Attorney General Neronha ended the summit with a fiery speech in defense of keeping Roger Williams and Fatima Hospitals open to the public and against the out-of-state owners of the hospitals that he called “lousy.”
Both the Attorney General and Senator agreed that immediate action is required.
Senator Whitehouse presented an option for Rhode Island - applying for the AHEAD Program, which would transition the state into a value-based, annualized payment system. Value-based health care is about “interventions that offer doctors and hospitals financial incentives that, in theory, induce them to improve both components of health-care value — cost and quality” — most commonly through ACOs, “a group of doctors and hospitals that are ‘held accountable’ by a public insurance program (such as Medicare) or an insurance company for the cost and quality of medical services provided to a defined population.”
What does this mean? That doctors are to be paid for positive health outcomes, not by collecting fees for services. The idea is to incentivize doctors away from costly medical interventions and testing and into working with patients to achieve healthier outcomes. The only problem? There's scant evidence that value-based healthcare approaches work. [See: Value-based payment has produced little value. It needs a time-out.]
State Senator Linda Ujifusa (Democrat, District 11, Bristol, Portsmouth) openly questioned the value-based payment premise being put forth by Senator Whitehouse and Dr. Howard Schulman at the event.
“I'm just wondering if either of you can address the question of whether there is any evidence that value-based payment systems have been working anywhere,” asked Senator Ujifusa. “Another name for that is capitation and we have seen that that simply does not work because what you're doing is putting the burden on providers and patients when in fact there should be more pressure on the middlemen insurers.”
Instead of peer-reviewed papers showing efficacy, Senator Whitehouse and Dr. Schulman presented hearsay evidence and/or declared the efficacy of value-based payment systems to be unknowable - evidence be damned.
“This is an issue I've thought a lot about,” said Senator Whitehouse. “I don't have the doctor's experience, but let me offer one thought. First of all, the fee-for-service system - we have to get off of that. It just doesn't make sense. It requires enormous amounts of churn. It does not allow the physician to be rewarded for making decisions out[side?] of billable things. I remember a story of a provider saying we need to get this guy an air conditioner and a TV so that he'll stop being a frequent flyer in the emergency room. You can never get reimbursement for that. You've got to have a doctor who's invested in making that work for that patient. It turns out the patient was turning up in the emergency room because he was hot and he was lonely. It worked and the system saved a bundle just for giving a guy an air conditioner and a television, but you can't make an air conditioner benefit and you can't make a television a benefit.
“So getting off a fee-for-service and to value-based care opens up room for that kind of initiative beyond the specific elements that are fee-for-service-able,” continued Senator Whitehouse. “It also eliminates the incentive that a practice might have to run the meter just to churn, churn, churn, churn, churn, and drive up billings.”
Dr. Schulman went so far as to say that the savings from a value-based payment system might defy easy analysis. “...you just can't put a number on it in terms of someone that - like a good lawyer -you know it when you see it. It's hard to rank them or give them a number,” said Dr. Schulman. “That's part of the problem.”
Here’s the four-hour video. I’ve transcribed and edited the words of Senator Whitehouse and Attorney General Neronha below, and included the question put forth by Weayonnoh Nelson-Davies, Executive Director of the Economic Progress Institute (EPI), the only person in the conference to ask about the possibility of universal healthcare.
Senator Senator Whitehouse: I have long worked towards the goal of trying to make Rhode Island's healthcare system a model for healthcare delivery around the country. I had hoped that the Lifespan/Care New England merger would be the vehicle for moving forward and completing that work, but that was not to be. Even without that vehicle though, the work can and should go on and we have two important opportunities before us that I wanted to flag.
These opportunities won't last, by the way. There is a window in which they are real and then they're not around any longer so we shouldn't waste them. They're things that we have to do together or not at all.
One would be to look to the regulatory system and create a consensus health regulation to protect our Rhode Island-owned hospitals from predation from out-of-state and secure improved cooperation between our hospitals. It's very hard for them to talk to each other with lawyers looking over [their shoulders]. Once you're in the safe harbor of regulation you can have that conversation, and I think it's important. I remember when all the major bank headquarters left our state - the economic ecosystem that those bank headquarters supported fell apart as the jobs and the professional support moved to where the new headquarters were. Downtown hollowed out. Downtown Providence still has not recovered and a lot of civic leadership in Rhode Island was lost. There was a lot of pain and I don't want to see that replicated in our hospitals. We have to make sure that local control prevails.
I don't want to lose the initiative that comes from local control, nor do I want to lose the opportunity for system-wide improvements that are deliverable only through government-enabled cooperation by regulation. We could set firm terms for out-of-state acquisitions of hospitals and terms for in-state cooperation between and among hospitals. This can form a structure for continuing Rhode Island's progress towards a true, value-based, local, efficient, and cooperative healthcare system.
Many of us can remember when our big hospital organizations were not getting along with each other and many of us can remember when they were not getting along well financially. Now we have a window of sunshine while they are getting along with each other and financially [viable] and we should use that window to prepare, in the safe harbor of a regulatory environment, for stormy days that still may come. That's one opportunity.
The second opportunity is to use the AHEAD Program [All-Payer Health Equity Approaches and Development] and Rhode Island's application to it to improve our reimbursement levels. I worked very, very hard to undo the imputed rural floor mischief, which for those of you who lived through it, knew was a dramatic blow to hospital revenues driven by a regrettable decision out of the federal government that we were able to correct. That put Rhode Island on a better payment footing. Still, it solved only part of the problem. The persistent hole Rhode Island is still in, with lower federal healthcare payments than neighboring Connecticut and Massachusetts, is a persistent aggravation - an aggravation of decades that doesn't lend itself to an easy solution.
The AHEAD Program moves participants more clearly to full value-based, annualized payment with little pressure. It also allows us to set that value-based reimbursement commensurate with our neighboring states in our regional market - not based on past rates held back by the unfair fee-for-service system - but on regional rates. I know that the delegation will gladly put our shoulders on the wheel to use the AHEAD plan to get out of that funding reimbursement hole. I don't see any other escape vehicle from the fee-for-service hole anywhere on the horizon. This is an opportunity, and I want to submit to something other than decades more unfair Rhode Island payment levels.
A health hospital cooperation regulation and an AHEAD reimbursement success will each only come with a consensus. I repeat neither is going to work without consensus. The Rhode Island Foundation has been a particular force for good in this area as have Integra and Coastal, our high-performing ACOs [Accountable Care Organization]. Our unions are at the table with expertise and experience to bring to bear. The bad old days of warfare among hospitals and insurers are behind us and we have leaders in those organizations who well understand the triple aim.
If we pull together there is the chance of achieving a long-sought common good, a major move away from fee-for-service to value-based reimbursement that brings us out of our regional funding hole and [creates] a secure environment for hospitals to secure the cooperative environment that lowers costs through better care. I cannot guarantee that we'll succeed, but this moment of possibility may not last. Let's at least try.
Attorney General Peter Neronha: The first question you should reasonably be asking me is why does your Attorney General claim to know anything about healthcare? I have to say I was a prosecutor for most of my legal life, and it's not by choice that I have spent time [on healthcare] over the last five or six years. I've only spent time here because the work has been imposed upon us. I have six lawyers doing healthcare today. When I started, I had one doing it full-time and one doing it part-time. The work is there for us to do.
Whenever I see people in medicine give a presentation, they often give disclaimers, so I'm going to give you my disclaimers. I'm married to a primary care physician and I'm the proud father of a newly minted doctor who's about to do his residency in Chicago. So perhaps that impacts my lens, but I don't think so. Let me begin by saying this: I don't know a lot about the AHEAD program that Senator Whitehouse talked about. I did some reading that my team provided to me last night, but I know this: the application is due in August.
I see some nods around the room. The application is due in August, and I'd like to see a show of hands. Who thinks we're going to have that application done by August? Do we even know who in this room is charged with preparing the application? We should know. I know, but I would guarantee that many don't and many in the broader population don't. So let's put the AHEAD program over there until we can get our act together here and get our application in place. That's an eight-year program for eight states that, if we don't get our application in now, doesn't happen. Either we pick up our game now or that ship is sailed, okay?
But make no mistake, we need change.
Why do I say this? Do you know that right now we are in Superior Court in a closed hearing fighting to keep Roger Williams and Fatima Hospitals open? The courtroom is sealed. I hear a lot in this job about the need for transparency, but where is the outcry from the media about why that courtroom is sealed? I take no issue with Judge Stern sealing it, but where is the media that criticizes my office repeatedly for not being transparent when there is nothing more important than what's going on in that courtroom? In that courtroom is the future of Roger Williams and Fatima Hospitals, make no mistake. They're $24 million behind in their payments. Why? They don't care about those hospitals. If they could, they would close them. Had we not forced them to put $80 million in escrow four years ago, they'd be closed today. They're closing hospitals all over this country and the only difference is we have money in escrow to prevent them from doing that.
That is the definition of a crisis, folks. One of my six lawyers is a bankruptcy lawyer. Do you think that's a coincidence? … I hired a bankruptcy lawyer because I see insolvency events on our horizon and they can't wait for a report in December. By the way, if that report in December recommends doing the AHEAD program, that ship will have sailed before the report's done. That report's not going to be all that helpful, to the extent it recommends the AHEAD program.
Why are Roger Williams and Fatima in crisis? It's not just because they have a lousy owner - and they do. It's because structurally, in this state, we don't bring enough revenue into the system to allow hospitals like that to function and be in the black and invest back into the healthcare systems. I jumped up when John Fernandez, President and CEO of Lifespan, said he's operating a public hospital because I wanted to bring attention to the point that in any other state, his hospital and probably every hospital in this state would be supported by public funds. And what is the appetite for public funds for these hospitals? Zero.
I looked at my iPhone before I got up here. My iPhone is an iPhone 12. I don't think that's the most current model. It costs $800 and yet everybody has an iPhone or an Android device. Why? Because we think having our means of communication at our fingertips is incredibly important and we'll pay any price to get it, right? If they raise that iPhone price to nine hundred, twelve hundred, fourteen hundred, we're going to pay it because we want our iPhone.
We want a healthcare system. We want bright, shiny new hospitals. We want to get a doctor tomorrow if we don't feel well or if we need a neurologist... [You want to] see a neurologist? See you in six months.
I think Dr. Michael Wagner [President and CEO of Care New England] said, “If you don't know anybody, you're not getting an appointment.” That's true because I'm married to a primary care doctor. Let me tell you something about primary care doctors... I'm married to one. She's a trooper. She could have been a Marine. She's never complained in the 30 years that I've been married to her. I met her when she was a resident. She has never once complained and I've never seen anybody work harder. I like to think I'm in an office and have held offices where people like my team work pretty darn hard, but nobody works harder than my wife. She is on that computer every night of the week until 10. She's on it Saturday morning. I know Senator Ujifusa's husband Mark is a primary care doctor. We value these gatekeepers to our health system so much that you can't see any other doctor until you go through them. The idea is that they're going to manage your care and yet we pay them the least to manage all of those referrals. I will tell you, as somebody who has turned 60, I need a hell of a lot of referrals, more than I'd like.
Why can't Roger Williams and Fatima Hospitals make it? It's because they are a 70-30 Medicare and Medicaid payer versus 30% commercial. Now, Martha Wofford [President and CEO of Blue Cross Blue Shield of Rhode Island], is right. Commercial payments are the train that is trying to pull Rhode Island into the 21st century when it comes to our medical system.
I remember going on Newsmakers and Ted Nesi and Tim White asked me, “How do we get more revenue into the system?” I said, “Grow the economy” and they scoffed at me. Make no mistake, getting people out of Medicaid and onto commercial insurance is the vehicle by which we can begin to solve this problem - in part. But do we ever talk about the economy in the context of urgency and what it means for healthcare? Not until today. We've got a lot of people on Medicaid and Medicare. We're old and we are economically challenged.
And then, our rates are lower than our neighboring states so we've got a double whammy and we need to fix that problem. We need to grow our economy and we need to increase our rates, folks. The AHEAD program may well be a means to increase our Medicare rates, but if we can't get our application in on time and the ship sails for some period of years, how are we going to do that? What is our plan to leverage our Medicaid dollars? These are things we can do if we recognize the scope of the problem, and if you're not in the game, you don't see the scope of the problem.
Somebody said to me that maybe it wouldn't be the worst thing if Roger Williams and Fatima closed. This is somebody who is involved in government at a high level... We know that we can't close those hospitals. It's not just about the jobs. I know you guys care about your jobs, ... it's about the patients first. And John Fernandez and Mike Wagner have both told me they can't take the overflow so we have to fight and save those hospitals and how do we fight and save them? We get those Medicaid rates up, we get those Medicare rates up if we can.
The federal delegation needs to fight for that and I know that they will. We need to leverage our Medicaid dollars to every last dollar. And if we're not doing it, we need to know why... Prospect, Roger Williams, and Fatima have been going on for three years now. It's why the $80 million is in escrow. If it wasn't, they'd be closed and the day of reckoning would already be here. We can't wait until the end of the year.
I spoke to some emergency room doctors not long ago and we were talking about private equity in healthcare and of course that has driven this crisis when it comes to Roger Williams and Fatima, no question about it. I said to them, “It's going to take spectacular failure for people to wake up.” And I would argue, given the state of oral health with children, we are in a state of spectacular failure [now].
We wonder why Providence School children don't perform the way we'd like. Well, if you can't eat and you can't think clearly because your teeth hurt, is it any wonder? We need to fix those three components of our healthcare system and we need to do it now because if we don't, we are going to have a more spectacular failure... We are too fractured in our thinking. We are too siloed in our thinking and we don't sit around the table and talk to one another enough directly and honestly, even though that's a hard conversation... I urged you to be bold and you looked at me like I was nuts. God bless you.
You know what I said to Martha Wofford? I said, “Don't spend more money on healthcare when it comes to providers. Just reallocate it. Make Rhode Island a magnet for primary care doctors. Take a little from the specialists, and give more to the primary care providers. Rebalance how we pay.”
I don't know if we can do that or not. Martha would probably tell me 10 reasons we can't. But it's that kind of thinking that I believe can move us forward. What I know won't work is continuing to do what we do today.
So what can we do? Well, for one thing, the governor's group that is talking about planning our healthcare can invite my office to participate, because I would argue no one has done more in this state, in the last three years, in defense of healthcare than my office... When we're at the table, we advance the ball and I'll tell you what the best evidence of that is that I can name every one of you out there that does healthcare by name. You know me and I know you because you spend time in my conference room. And even though we don't always agree... we talk and it's through those conversations and moving the levers of government that we can move this ship forward, but we can't wait and we got to have urgency...
I'm going to leave you with one thing. The beginnings of the correction are reworking our state regulatory bodies… We've got OHIC [Rhode Island Office of the Health Insurance Commissioner] in one corner doing great work, but it's over there. We've got the Medicaid office doing great work, but they're over there... You're trying to move this ship and you don't have enough people and you need a champion to get those people because there's nobody more important than the Medicaid office and leveraging our federal dollars. So if you take the Medicaid office and you put it with OHIC - I know you want to be independent [but] we'll figure that out.
This is just my plan. It's never going to happen. Take the Department of Health and bring them to the table as a true regulator empowered and funded and built to do real healthcare policy so we're not always relying on the Rhode Island Foundation... to give us the data. The state ought to have that data... How can we analyze these issues if we don't have the data? Let's figure out how to get the data. Let's get in the room and figure this out.
The Lifespan/Care New England merger wasn't good for Rhode Island. It was putting two weak places together, which never would've worked, particularly with leadership that didn't have a vision as to how it would work. But we are now in a place where we have great leadership in this state with Dr. Wagner and President Fernandez and Aaron and others. We have a great labor perspective... that can inform the policy decisions we need to make right now to get this done. There are moments in our history that require urgency, direct speaking, and not being afraid to rock the boat... As a state, we can't afford to hold back. We are on the precipice of a disaster and the beginnings are there.
Roger Williams and Fatima are there but you can't find a doctor there. The children can't get their teeth treated. We can fix it, but we need a state of urgency. We need to understand what's real and we need to get in a room, not a room where we talk at each other like I'm doing to you frankly, but where we talk together... I love small businesses. I do. But we need to bring some big businesses in here too. We can do it. There's no better place to live. I dragged my wife here from New Jersey. She took over Dr. Wagner's panel at what was then New England Medical Center 30 years ago because she loved this state and she'll never leave it. Let's fix this. We can do it.
Weayonnoh Nelson-Davies [Economic Progress Institute (EPI)]: People have hinted [at] centering patient's experiences when we have these conversations, looking at the positive health outcomes we want at the end of the day. In addition to doing healthcare policy at EPI, I spent 10 years as a legal aid attorney working with providers on their healthcare team, representing patients with social determinants of health issues. At the end of the day, what are we doing to increase patient outcomes? ... [Also], what are your thoughts about universal healthcare opportunities and concerns?
Peter Neronha: Yeah, look, I think universal healthcare is something worth talking about, but we're nowhere near talking about that. What I worry about is that we're doing healthcare piecemeal without a strategy. We rely too much on reports. We wait for reports, they come out, they make recommendations... Do we follow through on those recommendations? Where do they go? One thing I neglected to say as we talked about equity in healthcare is it's always the poorest and communities of color that will suffer first. If our community safety net hospitals go [and] if you're white and wealthy, you'll get your healthcare. You may get it out of state. But there's a reason Roger Williams and Fatima have that percentage of Medicaid patients - because they're treating communities of color and they're treating the poor... Those safety net hospitals - we simply can't do without.



Senator Whitehouse is protecting the profits and gains of the already wealthy!
I can't stand that we're paying ridiculous money for healthcare and not getting proper diagnosis (for years)! I owe $2200 to Cranston for an ambulance ride last month! My PCP called an ambulance and the ER doctor was angry that I was there! He said she should have called a neurologist and I shouldn't be there! (That's the third time in 14 months that I been told this!) BTW, after 24 hours in the ER, I was finally in a room!
So, if we're bothersome to them when we seek treatment, why should they be rewarded further?
I'm glad that the merger was rejected by the AG because hospitals have cut services and doctors have retired. ERs are understaffed, the busiest hospitals are crowded with many hours waiting time!
We wait MONTHS for doctors' appointments causing additional suffering and stress!
If they can't heal you, they make more money on long-term care and can reduce office staff, maximizing profits. WTF are they being aided by Senator Whitehouse?
What happened to the governing principles of for the people, by the people?
I've been sick for more than 5 years. I've moved my care to Boston for a specific ailment and finally found a doctor that HEARS ME!
I called a nonprofit!
Jo
Boston globe had an article on exorbitant healtyhcare costs as well today here is what I wrote for the BG comments section
A hospital near my house is trying to expand. Because we, members of the community, tried to stop the last expansion, the hospital is holding community meetings. I asked if building the new addition would reduce the cost of healthcare, healthcare that is already unaffordable. The hospital folks did not know that answer. But we do. It will raise the cost of healthcare if the hospital expands. The hospital simply will not admit it.
Having spent much time over the last 15 years looking at the cost of healthcare it does not appear to me that anything in any of the bills in the MA legislature are going to actually reduce the cost of healthcare. These are bills to increase spending. Not to say small hospitals do not need the money, but increasing reimbursement rates simply cannot reduce the cost of healthcare.
The only thing that really increases life expectancy, which to me is the only real goal of a healthcare system, is a good public health system. Preventing cancer is cheaper than curing it. We have to prevent asthma, as there is no cure other than cleaner air. But we look at cures as healthcare, prevention as anti business regulation despite the old saying of an ounce of prevention is worth a pound of cure, something truer today than ever. Unfortunately poisoning people is good for business as you not only get to sell stuff that kills, but it also means more healthcare spending. Prevention means we do not sell toxic substances that can spread through the community, and no one needs the cure.
Until we start to move towards a public health focused system, we shall never have affordable healthcare, and of course the private healthcare system will never move towards prevention, so none of the measures being taken by the MA legislature are likely to actually reduce the cost of healthcare. Which means more people will die unnecessarily simply because healthcare costs too much.