Fact-checking Governor McKee’s 2023 Executive Order suspending the never-enforced minimum staffing law of 2021
"Many of the statements in Governor McKee’s executive order sound familiar because they are identical to those we’ve heard frequently from industry lobbyists in recent months..."
Late Friday, Rhode Island Governor Daniel McKee issued an executive order indefinitely suspending penalties for nursing homes in violation of Rhode Island’s never-yet-enforced 2021 Nursing Home Staffing and Quality Care Act. Many of the statements in Governor McKee’s executive order sound familiar because they are identical to those we’ve heard frequently from industry lobbyists in recent months, but that doesn’t mean they are accurate or relevant to the argument.
Let’s look at those claims:
WHEREAS since January 2020, 400,000 nursing home and assisted living employees have resigned nationally due to pandemic exhaustion and low pay;
MOSTLY FALSE: McKee doesn’t provide citations for any of his statements, but this one seems to be taken verbatim from a Politico article published in July of 2022 and quoted by industry lobbyists. The Politico article cites statistics from the Federal Reserve Economic Database, but it gets the numbers wrong. In January 2020, the number of “all employees in nursing and residential care facilities” was 3,366,600. In July of 2022 (when the article was published), the number was 3,028,200. That is a decrease of 338,400. In November 2023, the most recent date for which data is available, the number of “all employees in nursing and residential care facilities” was 3,229,000. That is a decrease of 137,600 employees. While it’s possible that 400,000 employees resigned, that would mean another 262,400 new employees were hired.
McKee’s error aside, it's undeniable that there's a significant healthcare workforce shortage, both at a national level and specifically in Rhode Island. Implementing wage increases and establishing career advancement opportunities are crucial initial steps toward addressing this issue, and must be our immediate focus.
47% of direct care staff in nursing homes in Rhode Island rely on public assistance. 38% live in or near poverty levels. Mark Parkinson, head of the AHCA/NCAL, in a recent webinar sponsored by the Gray Panthers of NYC, boasted that CNAs in the United States are “getting to a point where we’re close to a livable wage.” We’re going to have to do much better than “close to livable” to build the workforce.
Many nursing homes in Rhode Island (certainly the nonprofit and independent ones, and those with a larger percentage of residents relying on Medicaid) cannot currently afford the necessary wage increases, with nonprofit facilities like Linn Health and Rehabilitation in grave danger of closing in the next few months, and others surviving thanks only to their endowments. Robust Medicaid reimbursement increases are necessary and should be tied to quality measures, financial transparency, and staffing.
Refusing to enforce the minimum staffing law does nothing to help the nonprofit facilities most at risk, as they have consistently met and often exceeded the minimum requirements.
WHEREAS, Rhode Island nursing homes have lost over 2,000 employees since December 2019, and Rhode Island nursing homes have lost 20% of their workforce since 2020;
TRUE, FALSE, and IMPRECISE: The United States Bureau of Labor Statistics shows that the number of employees working in nursing and residential care facilities in Rhode Island has decreased from 17,800 in 12/2019 to 15,500 in 11/2023, a decrease of 2,300, or 8%. Since December 2020, however, the year referenced in the second data point above, the number of employees working in nursing and residential care facilities in Rhode Island has increased by 100, from 15,400.
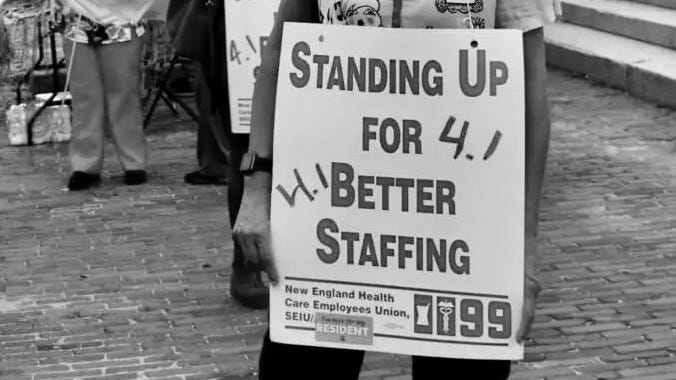
Regardless, the overall picture painted by these numbers is problematic. The solution, however, is to build the workforce, not to lower standards for the care received by nursing home residents, which we know declines when staffing is below 4.1 HPRD (hours per resident day).
WHEREAS, since 2012, Rhode Island nursing homes have lost more than $50 million in funding annually;
FALSE: Again, we know current Medicaid reimbursement rates are not adequate for nursing homes to cover costs for quality care, and we know that Rhode Island has not been following the 2012 law providing for inflationary adjustment, but one can arrive at very different figures for how much facilities have “lost” based on different methods of calculation, especially taking into consideration the various sources of pandemic-related aid. However, even the RIHCA doesn’t argue that facilities have lost $50 million annually, but rather in the eight years from 2012 to 2020.
WHEREAS, since 2020, six Rhode Island nursing homes have closed due in part to an unprecedented labor crisis;
MISLEADING: The Rhode Island facilities that have closed in recent years did so for a variety of reasons, the pandemic primary among them, but the workforce shortage was a minor contributor in most cases, and none closed because of the Minimum Staffing Law.
The workforce shortage is complicated by the fact that direct care workers can earn significantly higher wages working for a staffing agency than they can while employed directly by a facility, so facilities pay the additional wages, as well as the agencies’ cut. Additionally, many direct care workers regularly work significant overtime hours due both to inadequate staffing and inadequate wages, and this also increases a facility’s costs. (Both of these factors negatively impact patient care, as well.) While the workforce shortage does impact a facility’s bottom line, it is not a primary reason for recent facility closures.
Rather than working to solve the problems at the root of the labor crisis, McKee has short-changed long-term care residents by lowering the standards for their care.
WHEREAS three Rhode Island nursing homes have been placed into receivership in the last several months;
MISLEADING: The placing in receivership of Hebert Nursing Home, Trinity Health and Rehabilitation Center, and Pawtucket Falls Healthcare Center had nothing to do with the minimum staffing law or even financial difficulty.
Owners James Flanagan and Jeffrey Barnhill cited an “inability to pay debts” as their reason for filing for receivership for Hebert and Trinity, but this was after selling the real estate to a real estate investment trust (RIET) in 2017 that subsequently charged exorbitant rent ($1.9 million a year in rent for Hebert, valued at $5 million, and for which they were paid $8.9 million.) For Trinity, they realized a gain of nearly $14 million in just 3 years.
The companies certainly weren’t spending these profits on staff, as both facilities consistently had some of the worst staffing ratios in the state.
Pawtucket Falls was forced into receivership in May 2023 after a prolonged period of mismanagement and months of documented health and safety concerns. It has since been taken over by an out-of-state investor.
WHEREAS, since 2020, over 100 Rhode Island residents have been forced to relocate to different nursing facilities due to closures;
TRUE: And, over 100 Rhode Island long-term care residents in understaffed facilities filed official complaints (or had them filed on their behalf) for gross neglect during that time, as well.
WHEREAS, in 2021, the General Assembly passed R.I. Gen. Laws § 23-17.5-33, assessing penalties for nursing homes that fail to meet certain minimum staffing requirements (“Minimum Staffing Law”); and
TRUE, with great popular support, 34/38 yeas in the Senate, and 64/75 yeas in the House.
WHEREAS, the estimated net costs of enforcing the minimum staffing level compliance and enforcement program, pursuant to R.I. Gen. Laws § 23-17.5-33, would be approximately $60 million, further straining nursing home resources and potentially resulting in additional closures, and forcing the relocation of residents.
IMPRECISE/INCOMPLETE: Costs to whom and over what period? The total calculated for the second quarter of 2022 was approximately $11 million, and the top 78% of those unlevied fines would have been owed by eight mostly corporate entities. While the minimum ratio in the Rhode Island law increased as of January 1, 2023, national workforce numbers have also improved dramatically in the 21 months since the fines were calculated, making it less difficult for facilities to find staff to hire.
The bottom line: CMS studies and others have shown that 4.1 total HPRD [hours per resident day] (with various recommendations for specific CNA/RN/LPN hours within that total) is the minimum direct care staffing ratio necessary “to assure resident safety and attain or maintain the highest practicable level of resident well-being.” (See here and here.)
If we don’t require nursing homes to provide that level of care, we are sanctioning and ensuring unsafe and inadequate care for our most vulnerable population.
The imperative:
In tandem, we must:
Significantly increase Medicaid reimbursement rates, and those increases must be tied to thorough financial transparency requirements and multiple quality measures;
Enact a robust direct care worker minimum wage;
Reinstate the Safe Minimum Staffing Law.
Kathleen Gerard is with Advocates for Better Care in Rhode Island (ABC-RI)





Just wondering how it’s possible for the governor to “suspend enforcement” of a law. I’m assuming this law was duly enacted by the General Assembly and signed into law by the then governor (Raimondo or McKee?). Is anyone out there planning a legal challenge?
Thank you, Kathleen. Always good to know facts vs rhetoric when trying to understand important health care issues that involve our oldest and poorest RI citizens. Very sad commentary on how we value older sick people in this state. Just as poorly as we care for the homeless, or our school age children.